When a drug fails late on in clinical trials it’s a major setback for launching new medicines. It can cost millions, even billions, of research and development funds. Now, an ‘adaptive’ approach to clinical trials and a genetic tool for predicting success are increasing the odds of picking a winner.
When a drug fails late on in clinical trials it’s a major setback for launching new medicines. It can cost millions, even billions, of research and development funds. Now, an ‘adaptive’ approach to clinical trials and a genetic tool for predicting success are increasing the odds of picking a winner.
We all believe that the failure rate for drug candidates making it through phase III is unacceptably high. We want to be sure that we can answer the billion dollar question of which are most likely to be winners.
Ian Wilkinson
“Did not meet primary endpoint.”
Prosaic words, but they can mean a billion dollar failure has just happened.
The average cost of taking a scientific discovery all the way through to a drug on a shelf is enormous – last year it was estimated at $2.6 billion by the Tufts Center for the Study of Drug Development.
One reason the figure is so high is because it also includes the cost of failure. Recent years have seen some very high-profile failures of drug candidates that either did not meet the ‘primary endpoint’ (they didn’t work) or had their trials halted owing to serious side effects.
“It’s only natural that some drugs will fail in clinical trials – the process exists to ensure that treatments are safe and effective for patients,” says Professor Ian Wilkinson, Director of the Cambridge Clinical Trials Unit (CCTU) on the Cambridge Biomedical Campus. “But what’s unexpected is the high number of drugs that fail in phase III. You’d think that by this stage the molecule would be a sufficiently good candidate to make it through.”
He explains that failures in phases I and II – when the drug is tested for safety and dosage in healthy volunteers and patients – are inevitable. However, a great many molecules don’t make it through phase III, the stage at which the drug’s effectiveness is tested in large numbers of patients before regulatory approval is given. In fact only 10–20% of drugs that enter phase I are ultimately licensed.
“The problem with failing at phase III is it’s very expensive – a single drug trial can cost around $500m.”
He continues: “There’s a human impact for the thousands of patients who enrolled on the trial. For patients with cancer, it’s sometimes their last available treatment option,” says Wilkinson. “It’s also really unhelpful economically. Pharma companies have less money to put back into R&D, and it becomes even harder to fund drug development.”
This is why Wilkinson, along with a team of clinicians, scientists and pharmaceutical collaborators, together with statisticians at the Medical Research Council Biostatistics Unit, has been taking a hard look at the early phases of clinical trials. Their aim is to ask what can be done to get an early indication that a potential drug will make it to market.
“Traditionally, clinical trials have been organised to test safety first and efficacy last,” he explains. “It’s a cautious step-by-step approach adopted to ensure that pharma companies can satisfy regulators that the drug is safe.
“For many drugs this has worked well. But we are in a landscape where drug targets are more challenging – think for instance of conditions like psychiatric disorders and dementia. Leaving questions of whether a drug is effective to the final stages is now too risky and expensive.”
On any one day, the CCTU (one of the UK units accredited by the National Institute for Health Research) might be coordinating up to 20 trials in various phases for potential treatments for cancer, stroke, infections, dementia, heart attack, and so on.
Many of the trials are now designed with what Wilkinson calls “added value” built in at very early stages to give indications of whether the drug might work. This could include a biomarker that shows a drug for cirrhosis is reaching the liver, or a drug for heart disease is lowering cholesterol. “These are read-outs. They don’t show the drug works for the disease, but if the results are negative then there’s no point in progressing to later stages.”
The trials are also run ‘adaptively’. “We look at data for each person as it comes in… once we have enough information to guide us, we make a decision that might change the trial. It’s a quite different approach to the traditional rigidity of trials. It maximises the value of information a trial can yield.”
In recent years, pharmaceutical companies like GSK and AstraZeneca (AZ) have championed the need for rigorous trial design to weed out likely failures earlier in the process.
GSK has its only trials unit in the UK in the same building as the CCTU. There, GSK researchers work alongside Cambridge clinicians and scientists on first-in-man studies. A more targeted approach to testing medicines in patients is a key component of a Strategic Partnership between GSK, the University of Cambridge and Cambridge University Hospitals NHS Foundation Trust (CUH), which has the long-term ambition of jointly delivering new medicines to patients in the next five to ten years.
A few years ago, AZ analysed its drug pipeline before embarking on a major revision of its R&D strategy to increase the chance of successful transition to phase III and beyond. One area AZ identified as being crucial to success is to identify a causal relationship between target and disease. This might seem obvious but so-called mistaken causation has led to late failures right across the drugs industry. The usual cause is confounding – where a factor that does not itself cause a disease is associated with factors that do increase disease risk.
Professor John Danesh and colleagues at the Department of Public Health and Primary Care have pioneered a new way of finding evidence for causality before a patient is ever involved. Called ‘Mendelian randomisation’, it’s akin to a trial carried out by nature itself.
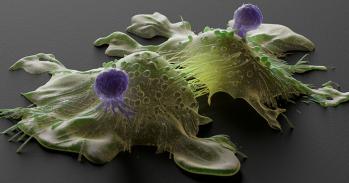
“Misinterpreting correlation as causation is a big problem,” explains Dr James Peters, who works with Danesh. “An increase in a protein biomarker in patients with atherosclerosis might suggest it’s important in the disease, but it’s not a valid drug target unless it plays a causal role. The conventional way to test this is to block the protein with a drug in a clinical trial, which is expensive, time-consuming and not always ethical.
“In phase III trials, the randomisation of participants helps to average out all differences apart from whether they are receiving the drug. Instead, we take advantage of the natural randomisation of genetic variants that occurs during reproduction.”
Some genetic variants can increase or decrease certain proteins that have been linked to a disease. If these variants can be identified – by computationally analysing enormous genetic datasets – then researchers can compare groups of people to see whether having the variant also increases the risk of a disease.
The team has used this method to look retrospectively at why two phase III trials for a potential cardiovascular drug failed. “The genetic evidence showed that the drug target was not valid,” says Peters. “We would have advised against taking this drug to a clinical trial.”
But it’s not just about predicting failures, Danesh’s team is picking winners. Evidence for the role of an inflammatory protein in atherosclerosis has now resulted in a clinical trial to see if an arthritis drug can be repurposed for atherosclerosis.
The researchers are helping industrial collaborators to prioritise potential drug targets and predict side effects. They also hope to expand their capabilities to test large numbers of variants for different potential targets in an automated fashion – a high-throughput approach to therapeutic target prioritisation.
Meanwhile, Wilkinson is planning ahead to avoid a different type of limitation: expertise. “There is a lack of individuals trained to design and deliver innovative clinical trials, and this is now impacting on drug development,” he explains.
Last year, an Experimental Medicine Training Initiative was launched to train medics how to run innovative clinical trials. Wilkinson is its Director and it’s supported by the University in partnership with CUH, Cambridge Biomedical Research Centre, and AZ/MedImmune and GSK.
“We all believe that the failure rate for drug candidates making it through phase III is unacceptably high,” he says. “Less than one in a thousand molecules discovered in the lab make it through to being a drug. We want to be sure that we can answer the billion dollar question of which are most likely to be winners.”
Read more about research on future therapeutics in Research Horizons magazine.

The text in this work is licensed under a Creative Commons Attribution 4.0 International License. For image use please see separate credits above.