Together against prostate cancer
How a partnership of scientists, patients and industry could transform prostate cancer care
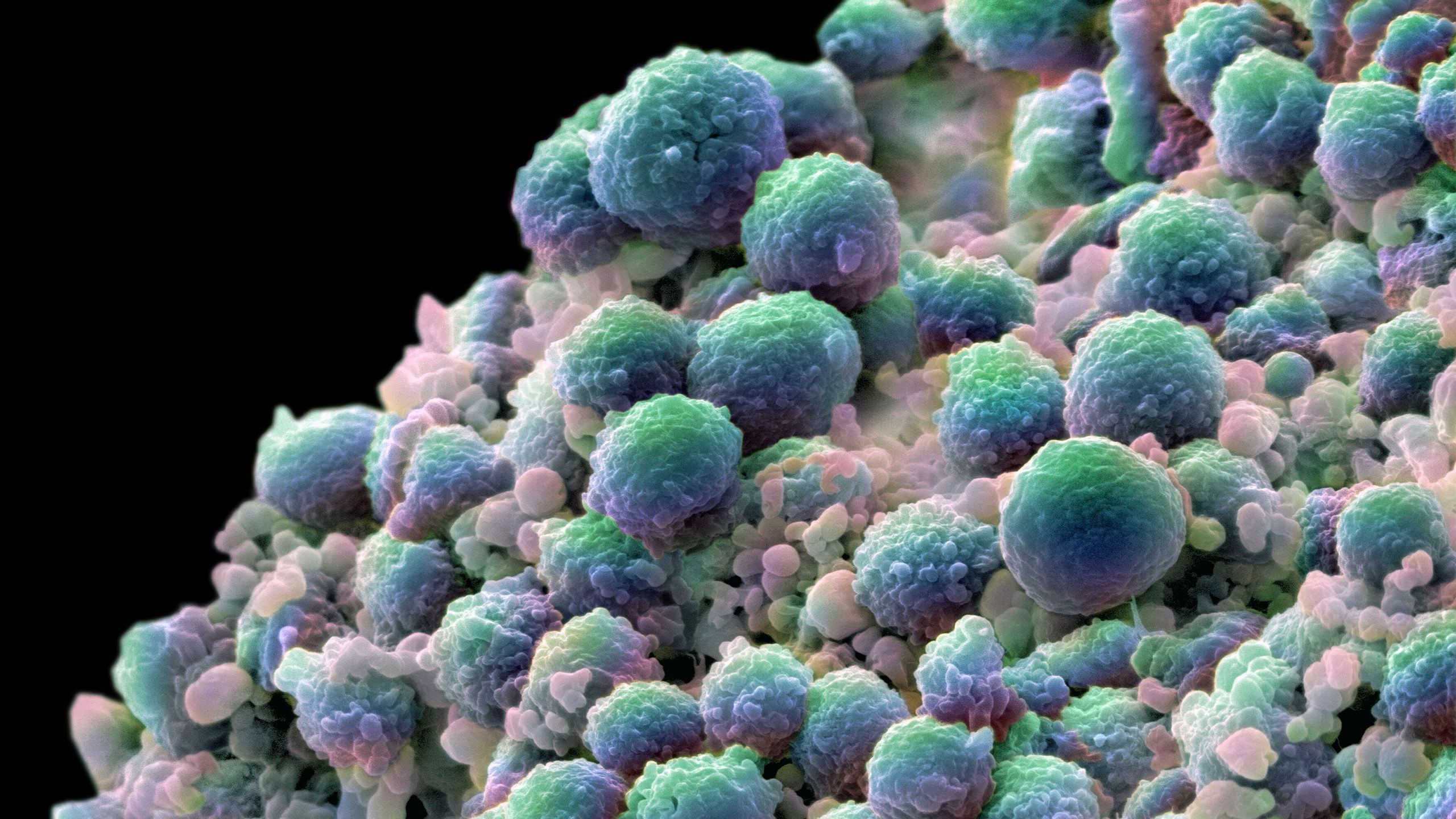
New, repurposed and combined treatments could soon transform prostate cancer outcomes, with DNA repair research informing promising clinical trials at Cambridge.
Prostate cancer is the most common cancer in men in 112 countries, and accounts for 15% of all cancers. Worldwide, 375,000 men died from the cancer in 2020. Only lung cancer ranks higher in terms of cancer mortality among men. The Lancet recently estimated that new cases will rise to 2.9 million by 2040 from 1.4 million in 2020.
The prostate gland sits at the base of the bladder. Cancers begin in the prostate’s lining epithelium and range from low-grade tumours that don’t require treatment to rapidly growing, lethal cancers. The biology behind this spectrum of cancer behaviour is only partially understood.
Andrew Pickering is raring to go. He’s young (not quite 61), fit and has a busy life being a self-employed interior design consultant, as well as being married with three sons and three grandchildren. But a few months ago, he had surgery for prostate cancer and he’s been forced to rest.
Men like Andrew hold vital information to change the story of prostate cancer for good. But men in his position aren’t always keen to take part in clinical trials, less because they fear side-effects, more because it’s one more thing to think about, and they don’t want to delay getting back to normal.
When he was invited, Andrew immediately agreed to take part and has no regrets. “There are limited numbers of people who can go on these trials. I felt it was the right thing for me to do. It's no good just having things in a laboratory. We need to try out treatments in people. It was no hardship at all."
“It was made clear to me that I wouldn’t benefit personally. That’s fine – if it can help people in the future, then great. I hope my sons never get cancer, but I wanted to support the research that might help them if they ever did.”
Andrew Pickering
Andrew is part of ASCERTAIN, a study which is investigating the biological effects of a new PARP inhibitor, an existing hormone treatment, and a combination of the two, on men with newly diagnosed prostate cancer.
For Andrew, this meant taking a pill once daily for three weeks between his diagnosis and prostatectomy. He has also been undergoing ECG, blood and urine checks since his operation at Addenbrooke’s Hospital in Cambridge.

Andrew Pickering with his wife Claire
Andrew Pickering with his wife Claire
ASCERTAIN is one of a number of ‘window-of-opportunity’ prostate cancer studies being run collaboratively by two University of Cambridge teams in partnership with AstraZeneca. It’s a multinational study involving colleagues in Europe, North America and Australia, with Cambridge as the joint lead.
These studies collect tumour biopsies before and after the investigational treatment to identify any impact on cancer cells of giving one or more drugs. At the same time, the researchers carefully assess patients for any side-effects.
Central to this work is the partnership of two teams led by Dr Harveer (Harvey) Dev and Dr Simon Pacey. Dev is a urologist, surgeon and lead for a surgical translational research group at Cambridge’s Early Cancer Institute. Pacey is a medical oncologist and an experienced investigator in early drug development. Both represent the University of Cambridge’s Department of Oncology, Cambridge University Hospitals NHS Foundation Trust, and Cancer Research UK.
Together, Dev and Pacey aim to exploit genetic vulnerabilities in prostate cancer to redeploy existing treatments and help develop new drugs.
Attacking cancer's Achilles heel
DNA repair is so important to our cells that we have evolved several methods of repairing damage. One of these involves an enzyme known as PARP, but there is a backup process known as homologous recombination that steps in should this method fail.
Cancer cells that harbour genetic alterations such as BRCA1 or BRCA2 mutations are unable to carry out homologous recombination. Cambridge scientist Professor Sir Steve Jackson realised that inhibiting PARP in these cells meant they had no way of repairing themselves and they would die off – he had found their Achilles heel.
“This really is one of those golden bullet therapies which target the cancer cells and spare the healthy cells around them.”
Harvey Dev
The benefits of PARP inhibitors for patients with BRCA and other mutations are well known, but Dev and Pacey’s work suggests that these benefits could be increased and more surprisingly, extended to the far larger group of patients who do not have homologous recombination repair gene defects.
In their previous work, Pacey and Dev have assessed the effects of giving an approved potent inhibitor of PARP enzymes, to patients for two weeks prior to prostatectomy. Half of these participants were also randomly allocated to an anti-androgen hormone treatment, which lowers testosterone levels. Analysis of biopsy and prostatectomy samples showed that inhibiting PARP enzymes contributes to a significant impact on the cancer cells even in some patients with no known gene mutations such as BRCA2.
The researchers found molecular evidence of drug effect in prostate cancer cells. The study also revealed several unique effects of combination treatment that were not as strongly observed with the PARP enzyme inhibitor alone, or in a separate study involving anti-androgen therapy. This includes changes in the expression of various pathways, including those involved in cell turnover and inflammation; these could help to explain why the combination treatment may be effective in a wider group of patients.
Crucially, both experimental treatments were well tolerated by all participants and had no impact on their planned operations or subsequent recovery.
NICE (the National Institute for Health and Care Excellence) recently approved the utilisation of the PARP enzyme inhibitor with drugs that block testosterone effects in patients with metastatic prostate cancer. Dev and Pacey want to understand this better and to see if the treatment could be repurposed at earlier stages of prostate cancer, to help many more men.
“Why would individuals without those DNA repair gene defects benefit from a therapy that works entirely through that mechanism? That’s what our lab is working on.”
Harvey Dev
“We’re interrogating the genetic drivers that underpin these processes and we've identified a few candidates that we think are important. We’re looking into novel markers which could be unrelated to the cascade of functions that BRCA is involved with but which we think are functionally relevant to how these drugs cooperate.”
The androgen receptor, the main hormone driver in cancer cells, is somehow contributing to the DNA repair process and it is through the combination of targeting that pathway and boosting the sensitivity of cancer cells to treatments that Dev and Pacey believe a breakthrough could be made.
Dev says: “As we start to validate our findings, we can go back to patients and look for those markers and see whether we've now identified another group of individuals who would benefit from combination treatment.”

Harvey Dev
Harvey Dev
The power of partnership

Simon Pacey
Simon Pacey
Pacey says: “For clinical trials to work best, you need collaboration with a translational lab like Harvey’s, critically supported by patients who wish to take part. Working with Harvey focuses the mind. We all have a shared interest in DNA repair and we’re looking for opportunities to convert discoveries in this area into developing effective treatments.
“We’re in a great place on this campus. It is quite unique that we can bring together surgery, radiotherapy, oncology, pathology and radiology experts to develop treatments for earlier onset patients to help them live much longer. And we’re right next to the biopharma company, AstraZeneca, which is world class at developing PARP inhibitors and DNA repair inhibitors.”

Cambridge Biomedical Campus
Cambridge Biomedical Campus
Pacey focuses his efforts on drugs in early development because, he says, they “offer a sweet spot to do something impactful in the lab and make a difference down the line for patients. I like what I do because the small scale of the studies makes it agile.”
Both Dev and Pacey can’t emphasise enough the importance of collaborating with trial participants like Andrew Pickering.
“We currently don't have great models for prostate cancer. The best model is human cancer itself."
Simon Pacey
"So we rely on these pre-surgical, window-of-opportunity studies. We rely on our patients giving us their time completely altruistically. My job is then to design a study to answer key questions while minimising the risk of side effects. I can’t get that risk down to zero but that’s what I’m aiming for so that men can undergo their planned surgery on time.
“We've got a really good track record in Cambridge of recruiting men to take part in these window studies, which is no small feat because the team might have to approach 200 men to recruit just 20.”
Andrew says: “During the trial you are monitored very closely. Even if the trial drugs had side effects or were found to be harmful in any way at all, I'm certain that it would be picked up very quickly and addressed. Having that attention is really reassuring. The care given by the doctors and nurses, who are working as part of the trial team, is second to none.”
Dev adds: “Most of what we do wouldn't be achievable without patients volunteering for the benefit of others in the future. It hits me with every patient interaction that we need to work fast to make a clinical impact now, rather than in 20 years’ time. This motivation really feeds into the very DNA of our new Early Cancer Institute. Physicists, engineers and mathematicians continue to make critical contributions to our research but we are also heavily and unapologetically clinical, and extremely aware of the need to accelerate our research efforts to help the very patients that we see every day.”
Fresh approaches
Both men are impatient for progress.
“Survival for later stage prostate cancer has improved due to new drugs being approved,” Pacey says, “but there’s a lot of room for improvement because men still aren’t living that much longer, compared to progress in some other cancers.”
“We now have the cellular and molecular technologies to look at cancers in much better detail but we’re not doing enough of that for prostate cancer yet. We’re five to 10 years away from having a lot more information than we do now for each patient. And then I think prostate cancer will move from a one-size-fits-all to increasingly be able to segment patients as we do with other cancers and having more personalised approaches.”
Cambridge Cancer Research Hospital, expected to open in 2029, will be a natural home for these fresh approaches.
Dev says: “The aim with the new hospital is to bring clinical translational research to the frontline so that we can have a faster and greater impact on our patients. And at the same time, patients will be providing the samples which advance our research into, for instance, early signals of cancer.
“We’re currently building the business case for the nation’s first molecular prostate clinic for early cancers. In the first instance, our vision is to bring genomic testing to all men in the East of England who have a newly diagnosed prostate cancer because of BRCA and other mutations. They aren’t being evaluated right now because of limitations in the existing infrastructure.”
Andrew Pickering is back to work now.
“I'm glad to get back into my routine,” he says. “I never imagined I would get prostate cancer. I noticed that I was having to go to the toilet more often than I used to, but I just put it down to getting older. It was only when I mentioned it at a routine health check that the nurse suggested that it might not be old age, and that it would be worth getting my prostate checked. The rest is history and how I find myself here today!"
It’s a familiar story. What results from the research that he and others are now making possible may not be.

Support cancer research at Cambridge
Cambridge hosts a cancer research community responsible for globally significant breakthroughs and innovations.
Together we are changing the way cancer is treated. Our scientists will make discoveries alongside expert clinicians treating patients, drawing on the world-leading expertise found within the University and across the Cambridge Biomedical Campus.
We will find cancer earlier and treat it better. Join us.

Published 13 August 2024
Images
- Main image: Prostate cancer cells by Annie Cavanagh / Wellcome Collection)
- Harvey Dev and Simon Pacey by Lloyd Mann
The text in this work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License
